Part 3: How do I Prevent Pressure Ulcers?
Part 3: Mobilisation
Early mobilisation is an effective way of preventing pressure ulcers and this was seen in the PJ Paralysis incentive in 20181. This was initially a 70-day challenge, launched by England’s Chief Nursing Officer Professor Jane Cummings. The PJ Paralysis saw hundreds of hospitals across the UK take steps to ensure patients got up and dressed and took part in activities instead of being stuck in bed. In all, the campaign reported to have given back more than 710,000 days to patients, according to those behind the scheme. An evaluation shows it has led to reductions in falls, pressure ulcers and shorter lengths of stay, as well as improvements in patients experience of hospital care2.
The EPUAP3 recommends the following guidance for mobilisation:
- Develop a schedule for progressive sitting according to the individual’s tolerance and pressure ulcer response.
- Increase activity as rapidly as tolerated.
- Individuals on bedrest should progress to sitting and ambulation as rapidly as they can tolerate.
- Ambulation schedules may help offset the clinical deterioration often seen in individuals subjected to prolonged bedrest.
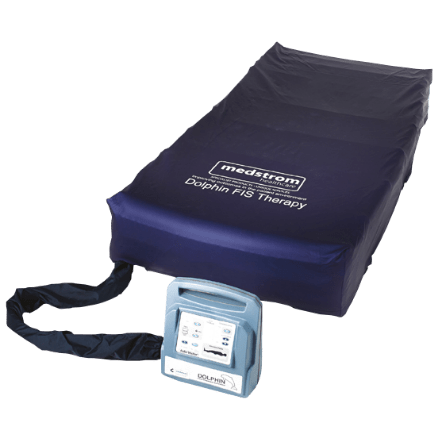
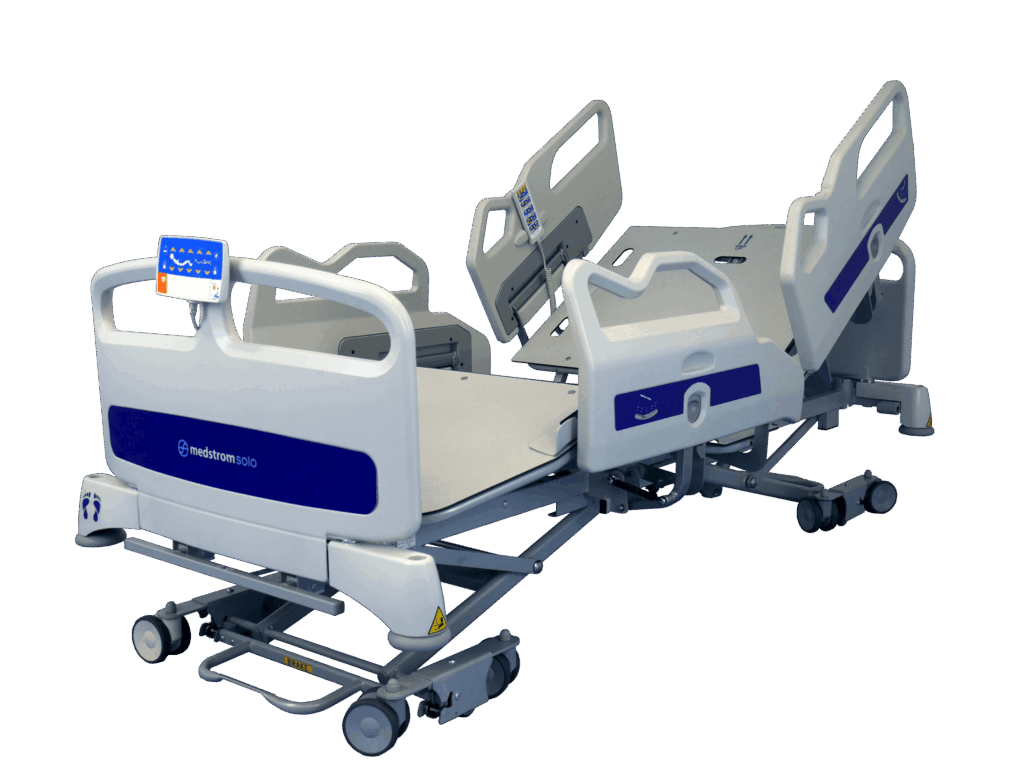
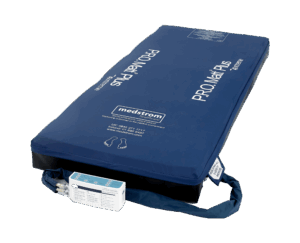
It’s also advised that if sitting in a chair is necessary for individuals with pressure ulcers on the sacrum/coccyx or ischia, limit sitting to three times a day in periods of 60 minutes or less3. Sitting is important to reducing the hazards of immobility, facilitating eating, and breathing, and promoting rehabilitation4. While sitting is important for overall health, every effort should be made to avoid or minimise skin damage and an appropriate seating surface and/or positioning techniques to avoid or minimise pressure on the ulcer. Medstrom have a range of pressure redistributing seat cushions to help with this aspect ( see Apollo 4 cushion), in addition a support surface protocol that acknowledges the need to ‘step down’ patients when they are mobilising from the bed (see Medstrom Aria).
In summary, there are adverse health outcomes associated with pressure ulcers. Pressure ulcers affect a patient’s quality of life, morbidity, and mortality. Once a pressure ulcer develops, complications such as infection with the potential for sepsis and death may occur. Christopher Reeve, (also known as Superman), died in 2004 following a pressure ulcer-related systemic infection that caused cardiac arrest5.
Therefore, there is a strong rationale for the early adoption of pressure ulcer prevention with the use of clinical judgement. Right product, for the right patient at the right time and “prevention is cheaper than care” (Judith Waterlow6) is an important Medstrom mantra that can help ensure patients and caregivers have access to the most suitable equipment when needed, rather than the transfer of a patient on to an alternative surface when their condition has deteriorated.
To read the rest of the series please click the links below:
How do I Prevent Pressure Ulcers?
Pressure Ulcers: Everything You Need To Know