Part 4: The Science of Surfaces Series
Part 4: How do Pressure Ulcers Form?
Moisture
In part 3, we looked at the effect of shear/friction on the skin. In this instalment, we will now look at moisture.
Skin can experience exposure to various bodily fluids such as urine, faeces, exudate, sweat or a combination of these at times creating a moist environment1. If the skin is exposed to these for a prolonged period, the skin can become wrinkled and soft, leading to saturation causing a higher susceptibility to friction damage and development of pressure ulcers1.
One of the key roles of healthy skin is to provide a natural barrier to prevent bacterial infections1. However, if a patient is incontinent of urine, the urea from the urine can change the skin’s environment, promoting bacterial growth1. Faecal matter contains enzymes that breakdown the skin’s barrier allowing for bacterial growth1. Incontinence of urine and/or faeces causes the natural pH of the skin in contact to change causing redness and breakdown. This irritation is known as maceration, excoriation or incontinence associated dermatitis1. Exposure to these bodily fluids can contribute to pressure ulcer development.
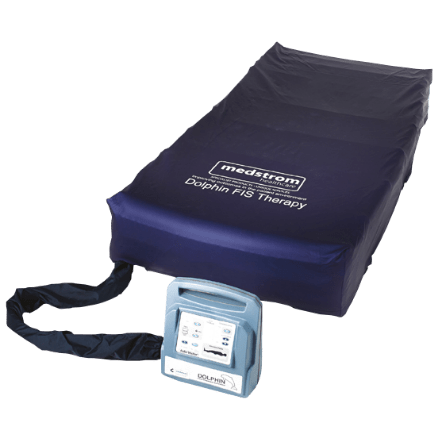
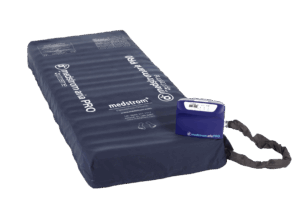
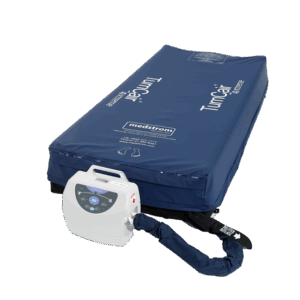
In terms of surface design, it’s important to consider the impact of moisture on the patient’s skin and use materials that can transmit moisture vapour (e.g., mattress covers with moisture vapour permeability characteristics). For plus-size patients, the impact of moisture could be increased due to increased perspiration. Mattress technologies such as low air loss (for example TurnCair 1000), are often more preferential for plus-size patients due to the cool air that can circulate underneath them.
Click the links below to read the rest of this series:
The Science of Surfaces
Part 1: How do Pressure Ulcers Form?